Irritable bowel syndrome: Using genes to predict whether a change in diet can help
European study shows that genetic defects in the breakdown of carbohydrates influence the extent to which people with irritable bowel syndrome benefit from a change in diet.
Irritable bowel syndrome (IBS) is a digestive disorder characterized by abdominal pain, bloating, diarrhoea or constipation. It affects up to 10% of the world's population. Despite its prevalence, the treatment of IBS remains a challenge, as the symptoms and response to dietary or pharmacological measures vary greatly. A European research team involving members of the Cluster of Excellence “Precision Medicine in Chronic Inflammation” (PMI) has now shown that dietary measures are more effective in IBS patients with defects in carbohydrate digestion genes than in those without these changes. They have published their findings in the journal Clinical Gastroenterology & Hepatology.
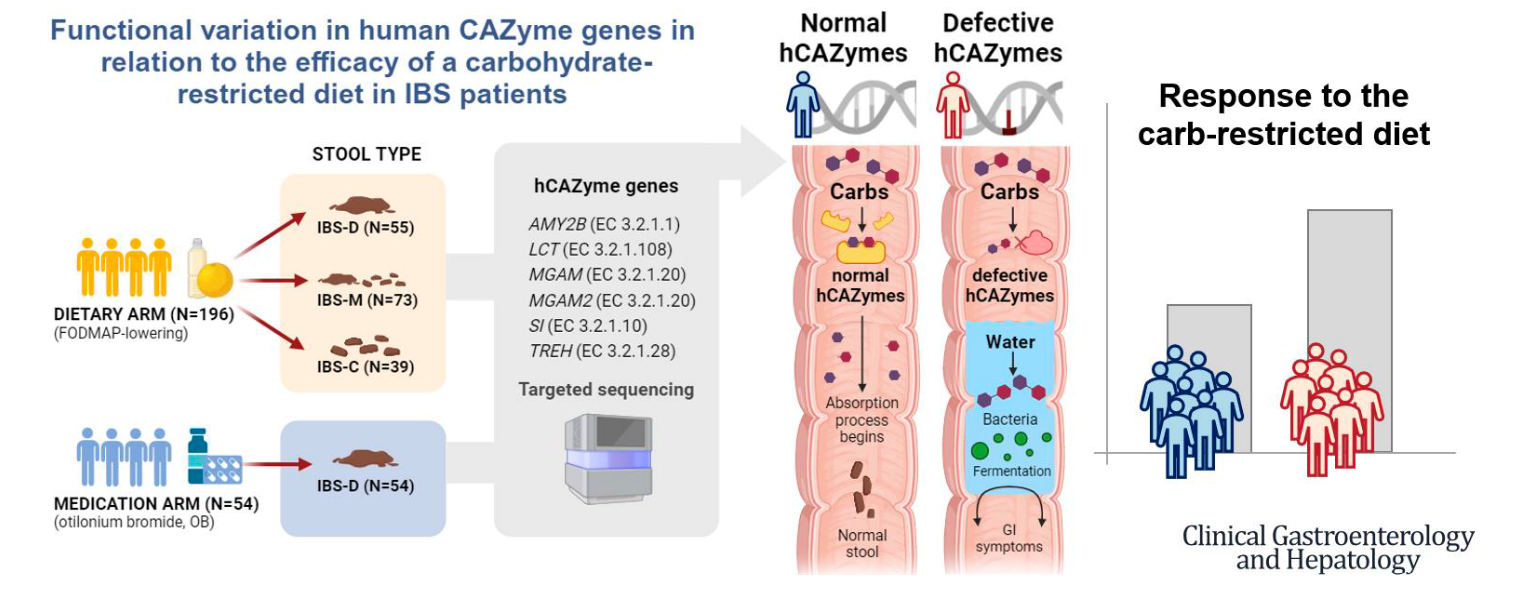
IBS patients often associate their symptoms with the consumption of certain foods, particularly carbohydrates. Avoiding these foods has been shown to be an effective treatment option, but not all sufferers derive the same benefit. Nutrigenetics - the science that studies the combined effect of genetics and nutrition on human health - has shown how changes in DNA can affect the way we process food. A well-known example is lactose intolerance, where the loss of function of the enzyme lactase impairs the digestion of dairy products. The work now published suggests that genetic changes in human carbohydrate-active enzymes (hCAZymes) can have a similar effect on how people with irritable bowel syndrome react to a low-FODMAP diet.
Research work involving the Institute of Clinical Molecular Biology (IKMB) at Kiel University (CAU) and the University Medical Center Schleswig-Holstein (UKSH), Kiel Campus, has investigated the role of hCAZymes in relation to irritable bowel syndrome. In a large-scale European research network, the GenMalCarb consortium, the team has now been able to show that people with defective variants in hCAZyme genes are more likely to benefit from a carbohydrate-reduced diet. In the study, which involved 250 patients with irritable bowel syndrome, two treatments were compared: a diet low in fermentable carbohydrates (FODMAPs) and the antispasmodic drug otilonium bromide. Of the 196 sufferers who took part in the low-FODMAP diet, those who were carriers of a defective hCAZyme gene showed a significant improvement compared to non-carriers. The effect was particularly pronounced in patients with predominantly diarrheic irritable bowel syndrome (IBS-D), who were six times more likely to respond to the diet. In contrast, this difference was not observed in patients receiving medication.
“The hCAZyme enzymes play a key role in the digestion of carbohydrates. Our results suggest that genetic variants of these enzymes could become critical markers for the development of personalized nutrition-based treatments for irritable bowel syndrome,” says Dr. Britt Sabina Löscher from the IKMB, co-author of the study and member of the Cluster of Excellence PMI. “In the future, knowledge of the hCAZyme genotype could therefore be incorporated into clinical practice and enable doctors to recognize in advance which patients are most likely to benefit from specific nutritional measures.”
This would not only avoid unnecessary restrictive diets for those who are unlikely to benefit, but also open the door to personalized medicine in IBS. The research team emphasizes that further studies are needed to validate these results and to understand the biological mechanisms involved. If confirmed, this approach could significantly improve the treatment of IBS and similar gastrointestinal diseases by making nutritional and therapeutic strategies more precise and effective.
The study involved researchers and clinicians from Spain (CIC bioGUNE), Italy (University of LUM and University of Naples), Germany (IKMB and University of Hanover), Belgium (TARGID) and the United Kingdom (University of Nottingham). The study was funded by the Spanish government MCIN/AEI/10. 13039/501100011033 (PCI2021-122064-2A), the German Federal Ministry of Education and Research BMBF (01EA2208B and 01EA2208A) and the Medical Research Council MRC (MR/W031213/1), under the umbrella of the European Joint Programming Initiative “A Healthy Diet for a Healthy Life” (JPI HDHL) and the ERA-NET Cofund ERA-HDHL (GA N° 696295 of the EU Horizon 2020 Research and Innovation Programme), the Spanish Government MCIN/AEI/10. 13039/501100011033 (PID2020-113625RB-I00), the German Research Foundation DFG (NA331/13-1 and 390884018) and the Belgian Health Care Knowledge Center (ref number: 16001).
Original publication:
Andreea Zamfir-Taranu et al.: Functional variation in human CAZyme genes in relation to the efficacy of a carbohydrate-restricted diet in IBS patients. Clin Hepatol Gastroenterol, 2024. https://doi.org/10.1016/j.cgh.2024.09.004
Scientific contact:
Dr. Britt-Sabina Löscher
Medical Faculty
Institute for Clinical Molecular Biology, Kiel university and UKSH
+49 431 500-15255
b.loescher@ikmb.uni-kiel.de
About the Cluster of Excellence PMI
The Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) is being funded from 2019 to 2025 through the German Excellence Strategy (ExStra). It succeeds the "Inflammation at Interfaces” Cluster, which was already funded in two periods of the Excellence Initiative (2007-2018). Around 300 members from eight institutions at four locations are involved: Kiel (Kiel University, University Medical Center Schleswig-Holstein (UKSH), Muthesius University of Fine Arts and Design, Kiel Institute for the World Economy (IfW), Leibniz Institute for Science and Mathematics Education (IPN)), Lübeck (University of Lübeck, University Medical Center Schleswig-Holstein (UKSH)), Plön (Max Planck Institute for Evolutionary Biology) and Borstel (Research Center Borstel - Leibniz Lung Center).
The goal is to translate interdisciplinary research findings on chronic inflammatory diseases of barrier organs to healthcare more intensively, as well as to fulfil previously unsatisfied needs of the patients. Three points are important in the context of successful treatment, and are therefore at the heart of PMI research: the early detection of chronic inflammatory diseases, the prediction of disease progression and complications, and the prediction of individual responses to treatment.
Press office
Cluster of Excellence "Precision Medicine in Chronic Inflammation"
Scientific Office
Head: Dr. habil. Susanne Holstein
Christian-Albrechts-Platz 4, 24118 Kiel, Germany
Contact: Sonja Petermann
+49 (0)431 880-4850
spetermann@uv.uni-kiel.de